Kiefer helps pave way for new therapies for inherited muscle disorders
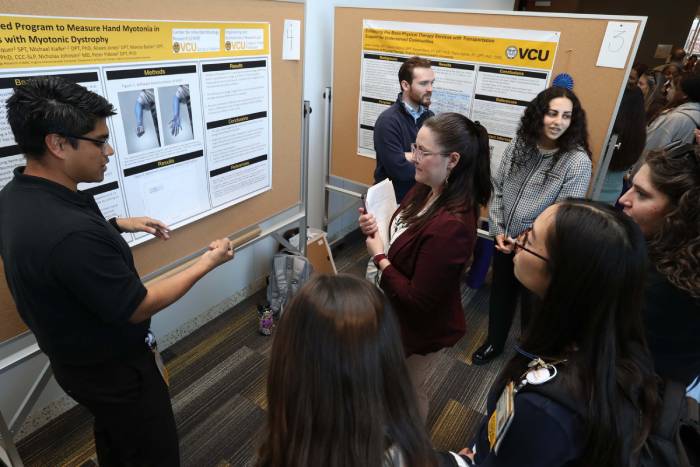
 At the intersection of clinical practice, scientific discovery and international collaboration, VCU physical therapy researcher Mike Kiefer, DPT, Ph.D., is helping rewrite the future for patients with rare and progressive muscle disorders.
At the intersection of clinical practice, scientific discovery and international collaboration, VCU physical therapy researcher Mike Kiefer, DPT, Ph.D., is helping rewrite the future for patients with rare and progressive muscle disorders.
With a background rooted in pediatric care and a growing research portfolio in neuromuscular disease, Kiefer is playing a key role in an ambitious international effort to validate new treatments for myotonic dystrophy, an inherited disorder that takes away muscle strength and movement.
“My clinical passion is pediatrics,” he said. “But my skill set is more broadly applicable to kids and adults.” That flexibility is critical in a field where symptoms often begin in childhood but evolve throughout a person’s life.
Kiefer splits his time between teaching in the Department of Physical Therapy and conducting research with the Center for Inherited Muscle Research, housed within VCU’s School of Medicine. The center, led by neurologist Nicholas Johnson, M.D., is a global player in the study of inherited muscle disorders, with a focus that ranges from gene therapy development to designing and coordinating large-scale clinical trials.
Kiefer’s expertise lies in what he calls a foundational – and often overlooked – part of that process: learning how to measure motor function in a way that makes clinical trials possible. “All of our foundational work tells us how to design that trial and how to measure if a treatment is effective or not,” he said.
For pediatric patients, that work is especially nuanced. “We have this upward trajectory of typical development for motor skills, and this downward trajectory of the disease that’s progressive,” Kiefer said. “The sooner you treat a condition that’s progressive, the more likely you are to have better outcomes…but it’s particularly challenging to measure because we have to account for children gaining new skills as they grow.”
His initial research aims to develop standardized outcome measures, which means clear ways to assess a patient’s movement over time. That might mean evaluating how a child rolls over, crawls or holds their head up – “every way that we can imagine to just test strength,” Kiefer said. “It’s figuring out which of those things are meaningful, and how do we say this is the measure that matters?”
Next comes understanding variability.
“Two people can have the exact same condition and have very different trajectories of motor gain or loss,” he said, noting that trial design must account for those differences so results are interpreted accurately. “We want to know: Is this person walking longer because the drug worked, or did they just have a more mild presentation of the condition?”
 Kiefer’s work feeds into multi-site, international consortia – one alone spans 22 sites globally – that track the natural history of disease. These study patients, who haven’t yet received treatments, are followed for years to better understand how their conditions typically progress, leading to baseline knowledge that is essential for assessing future clinical trials of gene or drug therapies.
Kiefer’s work feeds into multi-site, international consortia – one alone spans 22 sites globally – that track the natural history of disease. These study patients, who haven’t yet received treatments, are followed for years to better understand how their conditions typically progress, leading to baseline knowledge that is essential for assessing future clinical trials of gene or drug therapies.
The muscle disorders at the center of this work are complex and, historically, under-addressed. Myotonic dystrophy, one of the most prevalent adult-onset muscle disorders, makes it difficult for muscles to relax after contracting — affecting tasks as simple as letting go of a doorknob. Another focus of the center’s research, Limb-Girdle Muscular Dystrophy (LGMD), includes more than 40 subtypes that primarily affect shoulder, hip and trunk muscles.
Kiefer points to recent research that offers hope for effective treatments of these complex and rare disorders. “Spinal Muscular Atrophy had a breakthrough in 2016 that really changed things — children with severe impairments gained the ability to sit and walk in some cases,” he said. “While those aren’t curative, they show that there’s a real chance we can have a major impact.”
At VCU, researchers are working closely with pharmaceutical partners to bring similar breakthroughs to LGMD and myotonic dystrophy. “We have this true bench-to-bedside approach,” Kiefer said. Scientists study tissue samples and develop gene therapies, while clinicians like Kiefer assess patients in real-world settings to make sure the science translates to tangible improvements.
 Looking ahead, Kiefer is helping to train clinicians across sites to collect data consistently. “We want to make sure that the way I measure somebody’s muscle strength is the exact same way someone in California or in the UK does,” he said. “That’s a big piece of it.”
Looking ahead, Kiefer is helping to train clinicians across sites to collect data consistently. “We want to make sure that the way I measure somebody’s muscle strength is the exact same way someone in California or in the UK does,” he said. “That’s a big piece of it.”
And though clinical trials are underway, the work won’t stop there. “Even when there is, hopefully soon, an effective treatment, we’ll need new information,” Kiefer said. “As our treatments evolve, what we need to measure will too.”
His passion for the work is clear – sparked by a high school knee injury that led him to physical therapy, then deepened by time working with young patients at Cincinnati Children’s Hospital. What began as a goal of treating athletes shifted into a mission to help children with complex medical needs live fuller lives.
When asked what students should consider going into this area of clinical care and research, “It can be emotionally challenging, but it’s also really rewarding and a really exciting time. There’s a lot of enthusiasm and excitement about what the potential is for improving lives.”
by Kyra Newman